Pharma companies in India are under pressure to go beyond brand promotion and focus on real patient outcomes. Engagement programs, apps, awareness campaigns, and helplines are everywhere. But the real question is, are patients actually activated? Engagement means they’re listening. Activation means they’re doing something about it, such as filling prescriptions, showing up for follow-ups, or managing their condition proactively.
The distinction matters. Research shows that highly activated patients have a 31% lower risk of hospitalization and 24% fewer emergency visits compared to those with low activation levels. Another large study across 15,877 patients in England found that higher activation levels were linked to fewer GP visits and reduced A&E attendance.
For pharma, this translates directly into business impact: better adherence, stronger brand loyalty, and measurable ROI. Here’s a 10-step playbook tailored for Indian pharma to move from patient engagement to true activation.
Step 1: Start with clear definitions
Patient Engagement is the ongoing, two-way communication that helps people understand their condition, make informed decisions, and stay connected to their care. Patient activation is different: it’s the level of knowledge, skill, and confidence people have to manage their health on a day-to-day basis; the thing instruments like the Patient Activation Measure (PAM) quantify. Activation typically progresses in stages and, when it rises, outcomes improve and avoidable utilisation falls. Treat Patient Engagement as the engine and activation as the output you’re paid for.
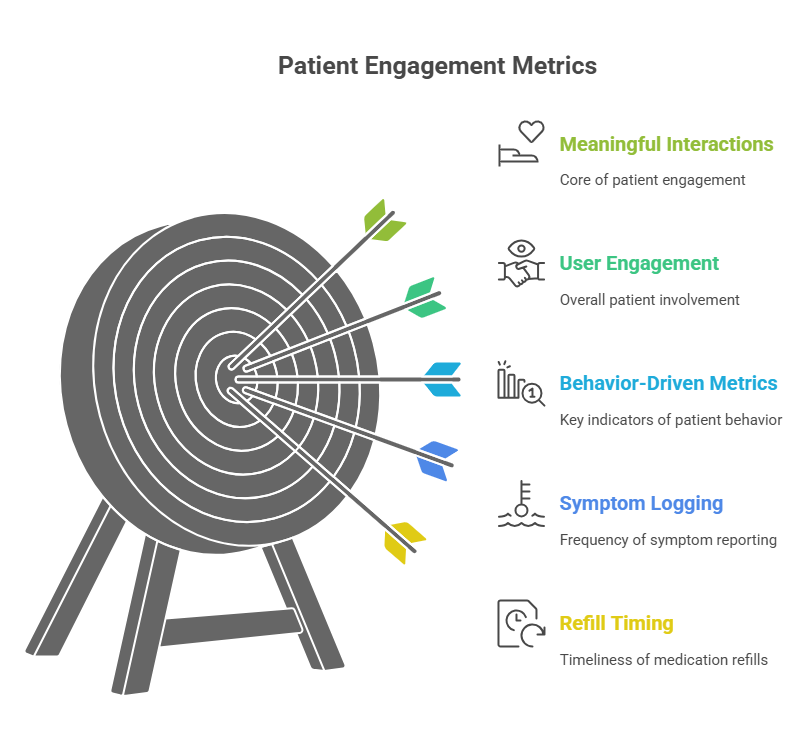
Define What You’re Measuring
Most pharma campaigns stop at engagement metrics: views, clicks, and impressions. That’s not enough. Activation needs to be measurable. Globally, the Patient Activation Measure (PAM®) is the gold standard. It’s a 13-item scale that classifies patients into four levels, from “disengaged and overwhelmed” to “maintaining behaviors and pushing further”.
If PAM isn’t viable in India due to licensing or cost, create proxies: refill adherence, time-to-fill, survey responses, or even repeat engagement with WhatsApp flows. The important part is to anchor your program in behavior, not clicks.
Step 2: Make patient activation a measurable objective
If you can’t measure it, you won’t improve it. Where PAM isn’t available, use proxies any commercial team understands: time‑to‑first‑fill, on‑time refills, persistence at 3/6/12 months, and completion of onboarding tasks. Track by therapy and region. Your review cadence should be monthly, not quarterly. Patient Engagement only matters if it moves people from passive to proactive.
Segment Patients by Activation and Risk
A one-size-fits-all program doesn’t work. Segment your patients by both activation level and risk profile.
- PAM Levels 1–2: Patients need high-touch interventions with field support, caregiver coaching, and vernacular voice flows.
- PAM Level 3: Chronic patients who benefit from regular nudges, such as WhatsApp reminders, and nurse-led check-ins.
- PAM Level 4: Self-driven patients who respond well to automated content and self-scheduling tools.
This ensures you’re not wasting resources on those who don’t need it, while focusing effort where the payoff is highest.
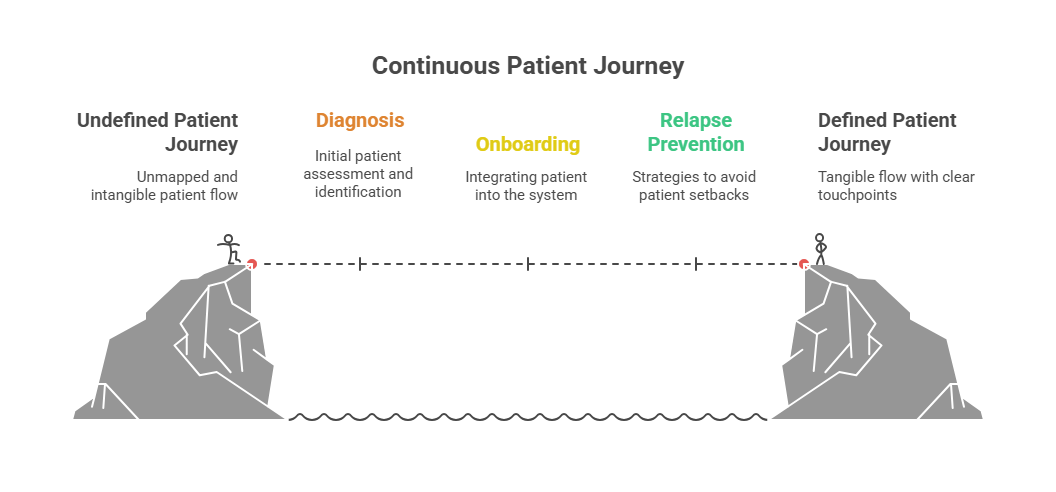
Step 3: Design a journey that doesn’t reset every quarter
Patients don’t live in campaigns. Map one continuous journey from diagnosis to sustained self‑management with clear checkpoints for education, onboarding, titration, relapse prevention, and lifestyle support. Connect that journey to your CRM so every interaction, whether clinic, call centre, WhatsApp, or portal, has context and an audit trail. In practice, this means wiring journey logic to your commercial CRM and regulated content libraries so nothing leaves the system without approvals and traceability. Patient Engagement wins when journeys are continuous, not episodic.
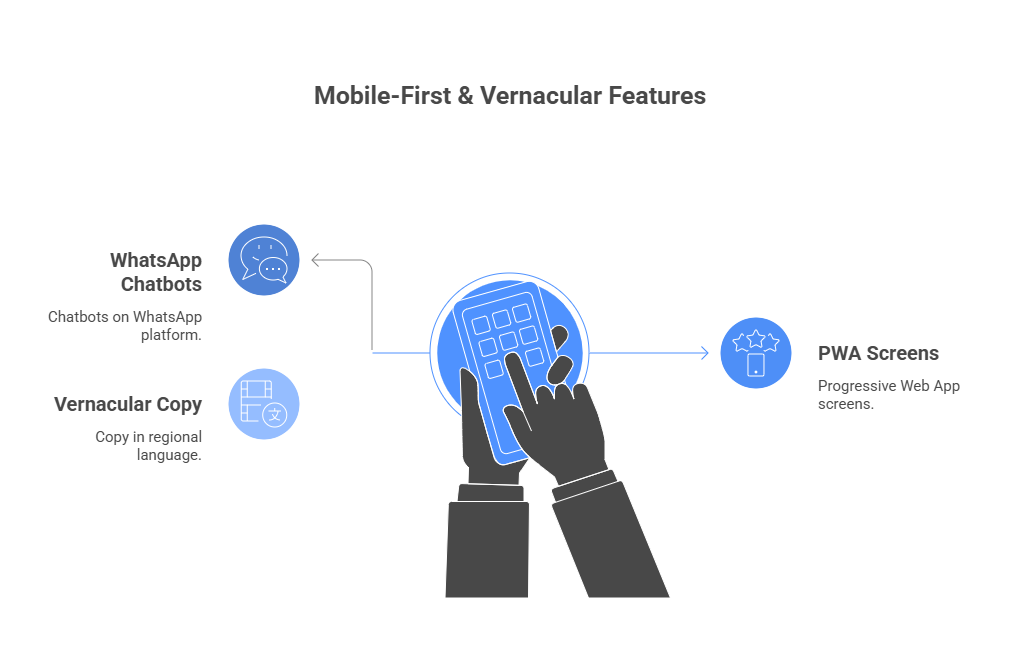
Make Digital Outreach Actionable
Digital tools can’t just broadcast, they need to drive measurable action. In India, this means using WhatsApp APIs, SMS, and Progressive Web Apps (PWAs).
Example flows:
- Prescription refill reminders with a one-tap confirmation.
- Short daily tips for lifestyle modification, linked to quick vernacular videos.
- Post-consultation FAQs delivered in local language via voice note.
Remote patient monitoring and digital reminders have already been shown to improve adherence, reduce readmissions, and cut outpatient visits. Pharma can bring this down to the patient’s phone.
Step 4: Go vernacular and mobile‑first
Activation stalls when content doesn’t fit people’s lives. Build low‑bandwidth PWAs, WhatsApp flows, and short explainers in regional languages. This isn’t theory. Indian programmes are already using WhatsApp chatbots to push prescriptions, diagnostic reports, reminders, and health updates at scale. Telemedicine expansions are training patients to complete follow‑ups digitally. Make actions dead simple: set a reminder, log a dose, ask a question, book a visit. Meet people where they already are.
Address Social Determinants of Health
In India, digital isn’t enough if you ignore social determinants of health. Low literacy, rural access, affordability, and even transport can derail activation.
Pharma programs should design for these realities:
- Use IVR voice calls in local languages for rural patients.
- Involve caregivers directly, since many patients rely on family for medication support.
- Offer financial counseling or connect patients to reimbursement schemes to reduce drop-off.
Ignoring these barriers means engagement campaigns look good on paper but fail in practice.
Step 5: Close the field-digital loop
Reps, nurses, educators, and your digital channels should speak with one voice. Give field teams the ability to trigger pre‑approved sequences right from their detailing or CRM screens so patients get the same message, the same day, in the same tone, and feed replies back to the rep and the brand dashboard. Field data shows that when channels are coordinated, reach and interaction quality improve. Build your stack so coordination is the default, not a miracle.
Build Cross-Functional Teams
Patient activation isn’t just a marketing job. In pharma, it cuts across medical affairs, digital, compliance, sales, and marketing. Programs succeed when these teams are aligned on objectives and share the same dashboards.
A practical approach: set up shared metrics (refill rates, PAM scores, engagement by region), hold regular cross-functional reviews, and ensure all patient-facing content passes compliance in real time through automated approval engines.
Step 6: Bake compliance into the workflow
Compliance is non‑negotiable in pharma marketing. Put medical-legal-regulatory review, consent capture, audit trails, and expiry controls inside the same systems that push content. Lock templates, localise safely, and log every outbound message. Under UCPMP 2024, transparency and ethics aren’t slogans; they’re table stakes. If compliance slows you down, your process is wrong. Done right, it’s invisible and absolute.
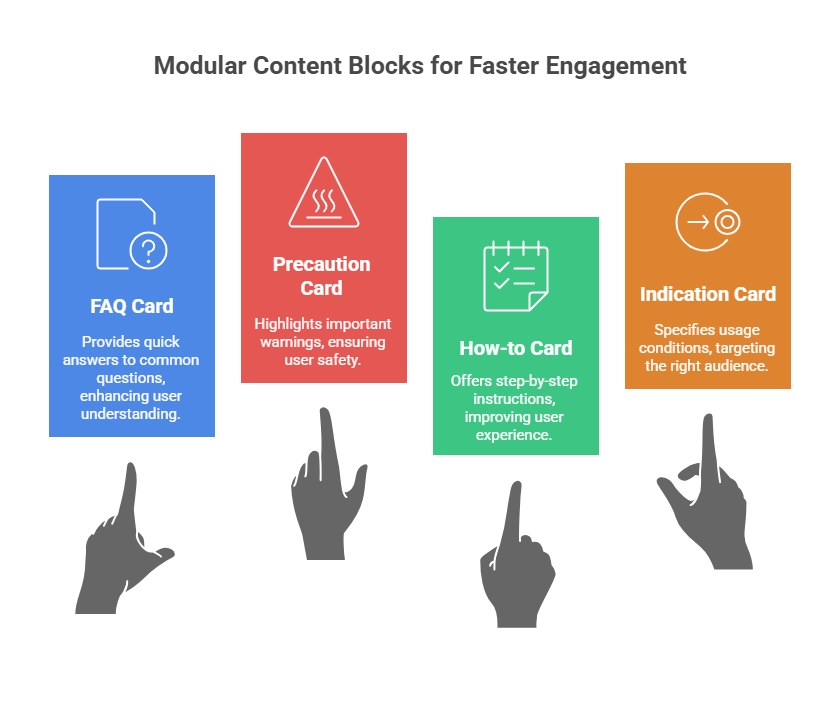
Step 7: Personalise with approved modules, not one‑offs
Personalisation only scales if it’s structured. Build a library of pre‑approved blocks, including indications, precautions, device how‑tos, and FAQs, that can be assembled per profile without fresh approvals. Use CRM/CDP data to decide language, format, and cadence. The goal is fewer review cycles and higher relevance. That’s how Patient Engagement becomes targeted without turning into a compliance nightmare.
Step 8: Measure what moves behaviour
Clicks are vanity. Track behaviours that signal activation: streaks in symptom logging, successful device demos, questions submitted to care teams, attendance at follow‑ups, and refill timing. Attribute those behaviours back to the touchpoints that drove them so budget flows to what works. Patient Engagement earns boardroom credibility when you can show behaviour change, not just open rates.
Keep Patients Engaged After the Visit
Activation doesn’t stop once the prescription is filled. Post-visit engagement builds trust and keeps behavior on track.
Ideas that work:
- Micro-surveys after pharmacy pickup (“Was the dosage clear?” “Any side effects?”).
- Educational nudges a week after prescription to reinforce correct use.
- Secure two-way messaging for patients to ask quick questions without waiting for the next appointment.
The feedback loop is crucial. Collect signals like confusion, side effects, and affordability, and route them back to brand or field teams to refine interventions.
Step 9: Build feedback loops after every clinical touch
Don’t wait for the next appointment to fix small problems. Post‑visit micro‑surveys and check‑ins surface barriers early, such as cost, side effects, and confusion. Route issues within 24 hours to a nurse callback, pharmacist counselling, or physician consult. Close the loop, then share de‑identified patterns with medical and brand teams monthly. Preventing drop‑off is the cleanest ROI story you can tell.
Tackle No-Shows and Therapy Gaps
Every missed refill or appointment is an activation gap. Digital nudges like appointment reminders, follow-up messages, and refill alerts can dramatically reduce these gaps. In some healthcare settings, reminder programs have cut no-shows by 14%.
For pharma, this translates into fewer drop-offs in therapy initiation and sustained adherence over time. Tie reminders to behavioral triggers: if a refill isn’t confirmed within 48 hours, escalate to a local field rep or helpline call.
Step 10: Prove it with a 90‑day pilot, then scale
Pick one therapy, three regions, two channels. Instrument everything. Define success on activation proxies and adherence, not pageviews. If thresholds are hit, scale; if not, fix content, cadence, or channel and rerun. Protect budgets, respect UCPMP, and build internal belief with evidence, not decks.
A 90-day pilot is the sweet spot. Pick one therapy, one geography, and one patient segment. Measure baseline adherence, engagement, and PAM scores. Then run targeted interventions and track uplift.
For example: “In a pilot with 500 diabetic patients in Tier-2 cities, WhatsApp flows improved refill adherence by 18% and raised activation scores by 10 points.” With that evidence, you can scale confidently across therapies.
Prove ROI with Outcomes
The ultimate test: does patient activation translate into better outcomes and business value? Evidence says yes.
- High PAM scores are linked to lower hospitalization and ER visits.
- In England, patients with higher activation had significantly fewer GP consultations and A&E visits.
- In practical terms, every 1-point increase in PAM score can translate to measurable reductions in healthcare utilization.
For pharma, the ROI is clear: improved adherence, reduced therapy drop-offs, and stronger patient loyalty. That’s impact you can take to the boardroom.
What this demands from your stack
You don’t need “more tools.” You need a CRM that talks to your messaging rails, an approval engine inside content creation, a CDP that unifies patient and HCP signals, and dashboards that link engagement to adherence and refills. You also need teams trained to trigger digital flows rather than fight them. This is execution work. Patient Engagement fails when tech is a patchwork and success is left to luck.
Lay Out the Tech Stack
Activation programs need a connected tech ecosystem. At minimum:
- CRM (Salesforce, Zoho, or equivalent) to manage patient journeys.
- Messaging platform (WhatsApp Business API, SMS gateway).
- Compliance approval engine for automated review of messages.
- Data lake for storing behavioral and PAM data.
- BI dashboards to track metrics by brand, geography, and segment.
Showing this stack signals to clients that you’re not just talking theory, you can execute.
Why this matters now
Indian pharma is rewriting the playbook. Patients expect digital clarity. Regulators expect discipline. Brands expect proof. The companies that treat Patient Engagement as a boardroom issue, not a side project, will outpace the market. They’re done with fluff. They need execution.
If you’re ready to move from good intentions to measurable patient activation, start by auditing your current engagement journey against these ten steps. The execution gap is where most programmes fail, and where the right partner can make all the difference.